Can Diabetic Retinopathy Be Reversed? – 4 Expert Tools
Reviewed by: Friedel Daniel, OD
We are grateful to Dr. Daniel for her expertise and contribution.
Here’s the thing about diabetic retinopathy: the damage is not reversible, but its progress is slow.
Here’s the catch: you won’t have symptoms until late in the game.
This means that you should catch the problem early if you do regular eye exams.
If you can catch the problem early, then you can prevent vision loss and even restore some of your lost vision (everyone’s mileage may vary).
You can prevent blindness or take steps to prevent any problems with your eyes.
So if you like seeing things in this beautiful world and if you want to protect your ability to see these wonderful things, then take some time to see the words of this article.
Key Takeaways
- Damage is permanent and cannot be reversed.
- You can regain some vision if you catch problems early.
- Symptoms might not appear before it’s too late.
- Regular eye exams are essential even if you have 20/20 vision.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. Always seek the advice of your physician or other qualified
health provider with any questions you may have regarding a medical condition.
What Is Diabetic Retinopathy?
First of all, what is diabetic retinopathy? More importantly, why should you care?
If we break down the word, we realize that constant high blood sugar can somehow hurt the eye’s ability to sense light.
Imagine a camera. You basically have a lens in front of a light sensor or film.
The lens will focus the light on the sensor. The sensor detects the light. Then you click a button to take a picture of the light on the sensor.
Similarly, our eyes have a lens and a sensor known as the retina. The lens will focus the light on the retina so that you can see the world clearly.
You cannot see the world clearly if retinal damage occurs.
In essence, you take a photo on damaged film; and we all know those pictures turn out fuzzy or white-washed.
If there is severe damage, then the retina cannot sense light at all. Simply put, you go blind.
So how does diabetes cause blindness? And can you reverse diabetic retinopathy?
How Does Diabetes Cause Retinopathy
Most people define diabetes as having too much sugar in the blood.
Having high sugar levels for a long time will defile the smooth lining of the blood vessels.
If there is enough degradation to the vessels, then blood flow is compromised.1 Oxygen and nutrients are not delivered effectively.
It’s like Amazon Prime. You can get 2-day shipping or next-day delivery only if the roads are well maintained.
If you have heavy traffic all the time (think rush hour, every hour of the day and night) then the roads will crumble fast!
So if your eyes are not getting their delivery on time, then the retinas have a potentially irreversible problem. In this case, a simple refund won’t rectify the issue.
The retina of the eye is energetically demanding. So the retina needs regular and consistent deliveries of nutrients and oxygen to support vision throughout the day.
If that supply starts to dwindle, then your eye will build new roads.
The catch?
The new roads are not well-made. They leak and crumble too easily.1
So the delivery trucks cannot make it to their destination easily or they lose their packages or the trucks get lost altogether!
Symptoms of Diabetic Retinopathy
There are no symptoms in the early stages.
Ironically, the early stages are where you can reverse any developing problems.
So annual eye exams are extremely important even if you have great vision.
Regular eye exams will help you catch or detect the early stages of retinopathy.
If you find them sooner, then it may be possible to prevent or reverse any damage.
These symptoms include but are not limited to:1
- Blurry vision – If you’ve ever seen a blurry photo, then you’ll know this frustrating experience. Imagine seeing the world as one big blurry photo!
- Visual distortion – What happens when you throw a rock into a pond or lake? Imagine seeing a world full of ripples and waves.
- Colors look faded or washed out – Remember how vibrant your favorite shirt was before you washed it hundreds of times?
- Dark floaters in your vision – Like dark, black clouds floating around in your field of vision.
- Vision loss – Lights out! Sudden and complete darkness of part or all of your vision (This is an emergency. Seek medical attention NOW).
How do you know if you should see the eye doctor?
Let’s talk about the risk factors.
Risk Factors for Diabetic Retinopathy
To protect your vision, we need to understand what threatens your vision.
The following is a small list of what can put your vision at risk.
You can proactively speak with your doctor about regular eye screenings to protect your vision.
Diabetes
- This one’s obvious. After all, “Diabetes” is in the name. Diabetes is the primary risk factor for diabetic retinopathy. There are two factors that makes diabetes dangerous to your eyes:
- Duration of diabetes
- The risk of developing diabetic retinopathy goes up with more time spent in a diabetic state.
- So frequent exams are important to find problems in their infancy.
- Poor blood sugar control
- As The Notorious B.I.G. once said, “Mo Money Mo Problems”.
- As The Notorious Dr. S.D. once said, “Mo Suga Mo Problems”.
- Duration of diabetes
High Blood Pressure
- Have you ever loosely attached a garden hose, and then watched it burst off when you opened the line?
- If not, then you’re smarter than me because that’s dangerous!
- High pressure on a fragile line can find weak spots.
- Ballooning or swellings can form (microaneurysms)
- Leaking fluid into the retina occurs (causing edema)
- The line may eventually burst (causing hemorrhage)
Cholesterol
- What happens when gunk builds up inside the ventilation system of your home?
- Airflow slowly drops (sometimes suddenly if that gunk breaks off and lodges itself somewhere).
- Less warm or cold air is being delivered to a room in the house.
- High cholesterol levels can cause plaque in the arteries.
- Blood flow slowly drops (again, sometimes suddenly)
- This will restrict blood flow to your eyes.
- Less blood flow means less oxygen and nutrients.
- Less oxygen and nutrients means the retina will start dying if a fresh blood supply is not delivered soon.
Pregnancy
- Every baker knows that slight alterations to a recipe yields dramatically different results.
- Extra sugar will affect the bun in the oven.
- The hormonal changes in pregnancy impact:
- Blood sugar levels
- Blood pressure levels
- You actually have 1.5 liters more blood when pregnant.
- More blood volume means higher pressure.
- These changes stress the blood vessels in the eyes.
Ethnicity
- Yes, ethnicity matters; and no one knows why.
- You are at higher risk of developing diabetic retinopathy if you are:
- African American
- Hispanic
- Native American
- This is not an exhaustive list.
- Regardless of your background, you should proactively screen your eyes if you have diabetes.
These are just a few risk factors.1
So speak with your doctor and be aware of your personal risk factors.
Regular eye exams give you the knowledge you need to make educated and health-conscious decisions.
Here’s what eye doctors look for when they gaze into your eyes.
Believe me, they’re not trying to be romantic.
Stages of Diabetic Retinopathy
The American Diabetes Association breaks the pathology into 2 categories and 4 stages.2
Category 1: Nonproliferative Diabetic Retinopathy (NPDR) or Early Stage
Stage 1 – Mild NPDR (Little or No Symptoms)
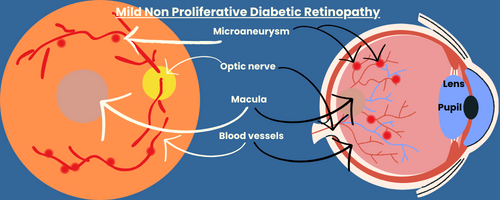
- Swelling blood vessels
- Normal blood vessels of the retina can develop tiny bulges.
- These bulges are known as microaneurysms.
- There are usually no symptoms at this early stage.
- Best caught with regular eye exams.
- Normal blood vessels of the retina can develop tiny bulges.
Stage 2 – Moderate NPDR (Low Risk of Permanent Damage)
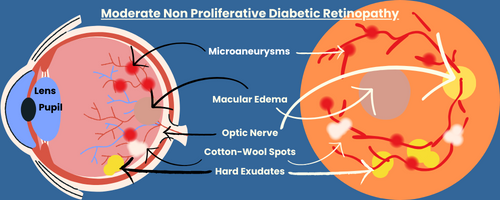
- Microaneurysms
- Blood flow likes to be nice and smooth.
- Microaneurysms form when blood vessels become more damaged by diabetes.
- These microaneurysms create a turbulent environment for the blood.
- Think of an airplane when it encounters turbulence.
- Turbulent blood has a hard time delivering oxygen and nutrients.
- Macular Edema
- Damaged blood vessels can also leak fluid into the retina.
- Excess fluid in the retina can lead to swelling.
- If the macula swells, then your vision can blur.
- This development is called diabetic macular edema.
- Symptoms include:
- Blurry vision
- Visual distortion
- Faded colors
- Cotton-Wool Spots
- Blocking blood flow will block the oxygen supply.
- Cotton-Wool spots look like swaths of cotton balls.
- They are thought to show where poor oxygen levels damaged the retina.
- This is permanent damage.
- No symptoms yet; but injury is building up.
- Hence, the need for regular eye exams.
- Hard Exudates
- These are protein and cholesterol deposits in the retina.
- These exudates will extract more fluid from the blood vessels.
- More fluid in the retina leads to more swelling.
Stage 3 – Severe NPDR (The Calm Before the Storm)
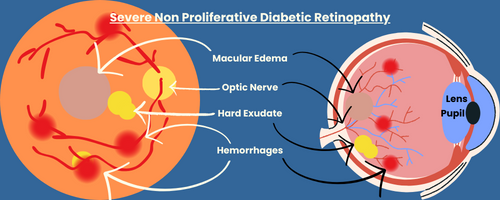
Stage 3 looks like Stage 2. However things are preparing to take a turn for the worse.
- Vascular Endothelial Growth Factor (VEGF)
- The retina needs oxygen and nutrients.
- Since the normal blood supply is compromised, VEGF is used to create new blood vessels.
- No new blood vessels are made yet; but the stage is set for significant problems soon.
Category 2: Proliferative Diabetic Retinopathy (PDR) or Advanced Stage
Stage 4 – PDR (Crazy New Vessels and Permanent Damage)
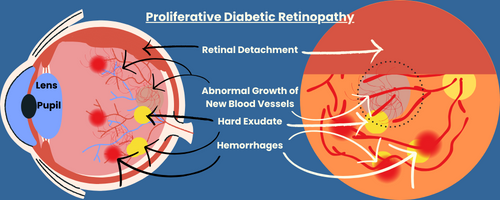
- Fragile and new blood vessels
- Since the original blood vessels are compromised or blocked, the retina needs new blood vessels to supply adequate amounts of oxygen and nutrients.
- Unfortunately, the new blood vessels are very thin and fragile. So they leak a lot.
- The leaks cause swelling of the retina and macula.
- The leaks can also lead to retinal detachment.
- This is called serous retinal detachment.
- Retinal detachment (An Emergency Requiring Surgery within 4 Hours)
- The back of the eye is rich with blood vessels that supply the retina.
- The retina loses all blood supply if it detaches from the back of the eye.
- The retina will die if it loses all access to oxygen and nutrients.
- Immediate surgery is necessary to restore the blood supply to the retina.
- The stakes? Permanent vision loss within 4 hours.
- Get treatment immediately if your vision changes suddenly.
Treatment for Diabetic Retinopathy
The name of the game is, “Prevention”.
Early detection is key. But what if you already have it?
Are there treatment options? Yes.3
Medical Control
Controlling blood sugar and blood pressure are paramount to your visual health.
If your A1C is less than 7.0%, then your diabetes is controlled.
If your blood pressure is less than 140/90 mm Hg, then your blood pressure is controlled.
Controlling these levels can help prevent more vision loss. You might even get back some vision because the swelling of the retina will go down.
Medicine
VEGF stands for vascular endothelial growth factor.
This stuff is like Miracle Gro for blood vessels.
If the body senses a need to create new roadways for blood to travel, then VEGF is created to promote the growth of new blood vessels.
There is a danger: overgrowth and sloppy jobs.
Leaky blood vessels can cause serious complications.
So anti-VEGF injections stop the growth of new blood vessels.
Stopping their growth will minimize risk of complications such as swelling and leakage in the retina.
Getting injections directly in the eye is cringe-worthy.
Although the thought is scary, people often say it’s like getting a flu shot in the arm.
The ophthalmologist does the procedure quickly and painlessly under local anesthesia.
Laser Surgery
When I think of laser surgery on the eye, I tend to think of magically seeing things clearly without glasses.
This is not Lasik surgery. Lasik addresses the cornea of the eye; which is the front of the eye exposed to the world.
When addressing diabetic retinopathy, laser surgery is used to identify and seal leaky blood vessels. By stopping the leak, we can reduce the swelling of the retina.
Vitrectomy
The eyeball is not filled with air; it’s not filled with water either.
The eye is filled with a kind of gelatinous goop known as the vitreous.
This goop can actually be removed to help you see better. Why does this work?
- It helps to remove any floating blood that is blocking light from reaching the retina.
- It can remove scar tissue so that the retina can be smooth.
- Repair a retina that detached from the back of the eye
The eye doctor specialized in this surgery will remove the goop (vitreous) and replace it with salt water (saline) solution.
Over time, your eye will replace that saline with natural vitreous humor.3
How to Protect Your Vision & Prevent Diabetic Retinopathy
Prevention is top priority.
Damage to the retina is often irreversible. So we must take steps to prevent injury before it begins and gets worse.
The following steps are cliché but paramount to your success.
- Diet
- Keep your diet on point.
- Regulate blood sugar levels in a normal range.
- Reduces harm to blood vessels.
- Improves blood flow to the retinas.
- Exercise
- Daily activity regulates blood sugar levels.
- Walking 30 to 45 minutes per day.
- Pro tip: Walk after meals (especially after dinner) to reduce blood sugar spikes.
- Medication
- Diet and exercise might not be enough.
- Your doctor may choose to prescribe medications.
- Control blood sugar levels.
- Control blood pressure.
- Control cholesterol.
- Yearly screening – Even if you think your vision is 20/20
- Yearly eye exams – Minimum.3
- To catch disease in the early stages.
- To take action before problems arise and become permanent.
- Yearly eye exams – Minimum.3
Can Diabetic Retinopathy Be Reversed? – Conclusion
So can diabetic retinopathy be reversed?
- Only if there is no permanent damage to the retina.
How do we prevent retinal damage; or at least catch it early in the process?
- Regular visits to your eye doctor; especially if you have no symptoms.
- Having no symptoms is the best time to catch any developing problems.
You can take action before it snowballs into disaster.
Always speak with your doctor to talk about your best options.
References
Find the references used in composing this article.

About the Author
Sami studied medicine with the fundamental belief that everyone is capable of making informed healthcare decisions.
He developed a desire to make medical information easier to understand so the patient can decide what is right for them.